As the bulk-billing debate continues to rage, DoHDA releases data showing just how many practices are, and are not, planning on shifting to full bulk billing.
Four leading GPs have laid into the federal government’s new bulk-billing incentive, saying it was designed for satisfying the optics of electoral politics, and not for supporting GPs, while the Department of Health, Disability and Ageing’s own data lays bare just how many GP clinics are planning to shift to full bulk billing.
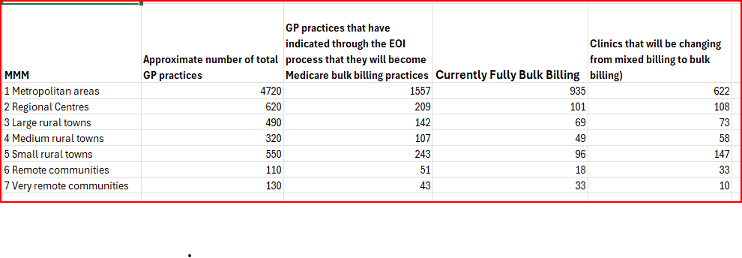
The data, sent to TMR by the Department this morning, was garnered from an expression of interest process designed to show how many GP clinics were planning on taking up the BBPIP by swapping from mixed billing to full bulk billing.
So far just 13% of 4720 metropolitan-based GP clinics who are not yet fully bulk billing (622) have indicated that they will shift from mixed billing as a result of the BBPIP.
Twenty percent of those metro clinics (935) are already bulk billing, says the data.
So far, a total of 1051 practices nationwide have let the Department know they are considering making the shift to full bulk billing. That’s in addition to the 1301 practices that have already made the move.
“I want every Australian to know they only need their Medicare card, not their credit card, to receive the health care they need,” said federal health minister Mark Butler.
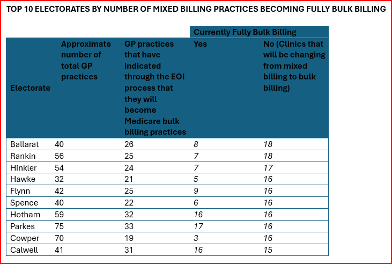
“Every electorate in the country will now have GP practices that bulk bill every patient.
Dr Karen Price, former president of the RACGP, Dr Mukesh Haikerwal, former president of the AMA, Dr Max Mollenkopf, a Newcastle GP and practice owner, and Dr Aniello Iannuzzi, chair of the Australian Doctors Federation, are unconvinced, to say the least.
Speaking in an ADF podcast last week, the quartet were scathing in their criticism of both the BBPIP itself and the government’s motivations for introducing it.
“I think [the BBPIP] has some use for those doctors who are already bulk billing in low socioeconomic areas, but it’s still a volume-based activity,” said Dr Price.
“It’s still related to high-volume throughput. We still haven’t addressed mental health. In fact, we’ve gone backwards. We haven’t addressed complexity and multi-morbidity. We haven’t addressed after-hours [care].
“And all it is, as I see it, is a quick fix for the politicians, and we’re still kicking the can down the road in what could be a genuine reform.”
Dr Haikerwal called the BBPIP a “smoke and mirrors exercise”.
“Many people have bought the lie,” he said.
“If [the government was] fair dinkum, they should say, ‘okay, this $8.5 billion, we’re going to try this, and if it doesn’t work, we’re actually going to not take that money out of health, but then cut it in different way and use it in a different way’.
Related
“The lie is that it all of a sudden $8.5 billion will be spent.
“It won’t be spent. The multiple tiers of complexity to the scheme and the yoking of general practice to this process is – by stealth and without any real money – trying to nationalise general practice,” he said.
“It’s easier to control if it’s done in this way, and that’s the problem. They don’t want to have a conversation with what has been the bedrock of our healthcare system, because they don’t like the inability to control what they see.
“This is a way of exerting control, nationalising on the stealth. You could make an argument that it is a kind of civil conscription, and what really concerns me the most is the people that work in our practices on the front desk are going to get hammered because of misinformation and expectation that cannot be fulfilled.”
As a younger GP and practice owner, Dr Mollenkopf said the federal government was not delivering on what his colleagues wanted and needed.
“My colleagues don’t want to be told that things are going to be free, when, in fact, they’re going to cost something because they don’t want to have to hose down expectations,” said Dr Mollenkopf.
“They don’t want to have to disappoint the people in front of them.
“They also don’t want to have to give up their own personal income, give up their own personal time.
“They would like to see a system where they can provide the care they need to for complex patients, while also providing fee-for-service care for those that can afford it.
“And they want more choice in the way they provide care.”
Dr Price said politicians were not interested in what GPs thought of bulk billing but in the optics of “free healthcare”.
“Bulk billing is a proxy. And I’ve said to the government, your proxy, it’s a wrong proxy. It’s not a proxy for us (GPs),” she said.
“They’re not talking to [GPs]. They’re talking to the patients. They’re talking to their electorates. They’re talking to what is a populist theory, because people find it hard to determine quality.
“We need to talk about clinical autonomy. We need to talk about the fact that our decisions for healthcare need to be free of government interference.
“The patient needs to know [that] with a so-called nationalist system or a bulk-billed system, the government is going to be in their room.
“It comes back to the government not respecting the professionalism of our profession and the high degree of training we have in Australia, and the high standards with which we perform our job.
“They have no idea, or they don’t care, one or the other.”





