The news from the ABS Patient Experiences survey was a ‘great sign’, said the RACGP president. Almost two-thirds could see their preferred GP when they needed to.
Fewer Australians are delaying healthcare than two years ago, according to new data released today by the Australian Bureau of Statistics.
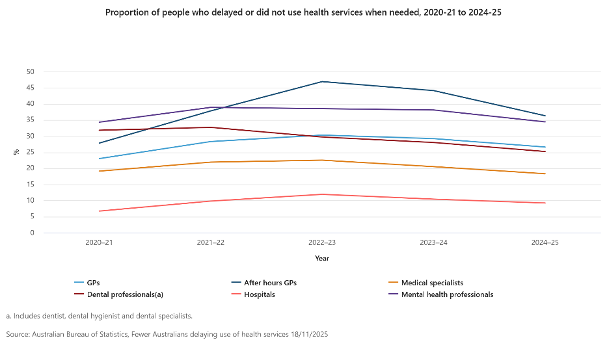
The ABS’ Patient Experiences survey revealed that in 2024-25 27% of people delayed or did not see a GP when needed – a 3% decrease on the 2022-23 figure (30%).
Similarly, 25% delayed or did not see a dental professional when needed, the lowest proportion since 2021-22 when 32.7% delayed dental care.
Eight percent of people cited cost as a reason for delaying or not seeing a GP when needed, while 16% considered cost a barrier to seeing a dental professional.
President of the RACGP, Dr Michael Wright, said the news showed access to GPs was improving.
“Nearly all Australians – literally 99% – can see a GP when they need to, and usually see their preferred GP,” he said.
“That’s essential. When you see a specialist GP who knows you and your history, you don’t need to start from the beginning. Your GP knows what you came in for last time, what medications you take and why, and what screening you should be doing to catch issues early. There’s no substitute for that care.”
Dr Wright also said the drop in people delaying GP care because of cost was a “great sign”, especially in the 15–34 years age group.
“Young people face higher costs at a time of higher mental health challenges, but good health at that age sets you up for a healthy life. It also reflects our recent Health of the Nation report – access to affordable GP care remains high,” he said.
“It’s also another datapoint showing GPs are spending longer with patients. The typical GP consult is now almost 20 minutes and has increased by 11% over the past three years due to more patients needing more complex care.
“It’s heartening that more patients are reporting their GP spends the time with them they need, but the patients less likely to report their GP spends enough time with them are in less-advantaged areas and live with chronic conditions.
“These are the patients who most need higher Medicare funding for longer consultations. Research consistently shows patients who can spend the time they need to with their GP are less likely to need hospitalisation.
“State-funded hospital systems are costing more and yet waiting lists and ramping remain, and patients repeatedly needing hospitalisation are a major reason why. Presentations to emergency departments are increasing by around 2.3% per year, and these are patients disproportionately from our most socioeconomically disadvantaged areas.
Related
“Emergency department wait times vary by state and hospital, but one thing is consistent – too many hospital beds are occupied by patients with chronic illnesses due to too little investment in preventive care by GPs.
“If we want a resilient health system and cost-effective hospital system, there’s a simple answer. Increase Medicare funding for long consults so patients can spend the time they need with their GPs.”
“The survey found that 65% of Australians living in areas of least socio-economic disadvantage saw a dental professional in 2024-25.
This compared with only 42% of people living in most disadvantaged areas.
After-hours GP care saw the largest decrease in delay of care, with 36.3% delaying care in 2024-25, compared with a record high of 46.9% back in 2022-23.
Fewer patients are delaying mental healthcare – 34.4% in 2024-25, compared to 38.1% the previous year.
The percentage of people delaying seeking help from a non-GP specialist has also dropped, from a high of 22.5% in 2022-23 to 18.3% in 2024-25.
Seeking care from a hospital has also seen improvement with just 9.2% of patients delaying care, compared with 10.4% the previous year.
Experiences of health services also differed by remoteness, said the ABS.
“Nearly one in two people (46%) living in major cities were seen by a GP for urgent medical care within four hours, compared to 30% of those living in outer regional or remote areas,” said the report.
“Less than one in four people (22%) used telehealth services in 2024-25, down from a peak of 31% in 2021-22.”