Healthcare workers who deal directly with patients have a more than three-fold higher risk of being hospitalised with COVID-19 than non-patient-facing healthcare workers.
Welcome to The Medical Republic’s COVID Catch-Up.
It’s the day’s COVID-19 news in one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
2 November
- Patient-facing healthcare workers have triple the risk of COVID-19 hospitalisation than non-patient-facing.
- Face masks do not reduce oxygen saturation levels in the elderly, study finds.
- Trump rallies may have led to additional 30,000 COVID-19 cases and 700 deaths.
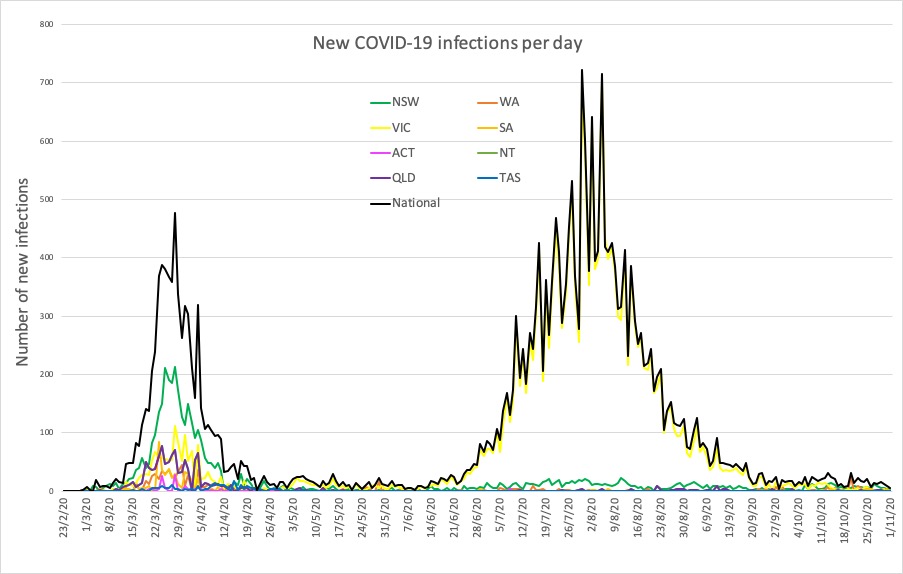
- Latest confirmed COVID-19 infection numbers from around Australia.
- Healthcare workers who deal directly with patients have a more than three-fold higher risk of being hospitalised with COVID-19 than non-patient-facing healthcare workers, and their housemates and families are also at elevated risk
A study published in the BMJ looked at COVID-19 hospitalisation rates among 158,445 healthcare workers in Scotland and 229,905 members of their households from 1 March – 6 June.
This revealed that the risk of hospitalisation was 3.3-fold higher among patient-facing workers compared to those not patient-facing. Among those who dealt directly with patients, those at the front door of healthcare facilities had double the risk again compared to other patient-facing workers.
Those not in patient-facing roles had a similar risk of COVID-19 hospitalisation as the general population.
The research also found that household members of patient-facing healthcare workers had an 82% higher risk of hospitalisation with COVID-19 compared to the households of non-patient-facing healthcare workers.
“Our findings from the ‘first wave’ in Scotland show that healthcare workers in patient facing roles—especially those in “front door” roles—are, along with their households, at particular risk,” the authors wrote. “These findings should inform decisions about the organisation of health services, the use of personal protective equipment, and redeployment.” - Face-masks have no effect on oxygen saturation, even in the elderly, a study has found. According to a research letter published in JAMA, the crossover study in 25 volunteers aged 65 years or old – one-third of whom had at least one comorbidity – found wearing a three-layer cotton non-surgical mask during normal activities had no impact on peripheral oxygen saturation.
“These results do not support claims that wearing nonmedical face masks in community settings is unsafe,” the authors wrote. - Make America More COVID-19-Positive Again? It might as well be Trump’s slogan, as a non-peer-reviewed study estimates that eighteen Trump rallies in the United States will have led to an additional 30,000 cases of COVID-19 and around 700 deaths.
Researchers from Stanford University looked at the county rates of COVID-19 infections before and after the Trump rallies, as well as accounting for COVID-19 control measures in those areas, and also used similar counties that didn’t host rallies as controls.
“Our analysis strongly supports the warnings and recommendations of public health officials concerning the risk of COVID-19 transmission at large group gatherings, particularly when the degree of compliance with guidelines concerning the use of masks and social distancing is low,” the authors wrote. “The communities in which Trump rallies took place paid a high price in terms of disease and death.” - Here are the latest confirmed COVID-19 infection numbers from around Australia to 9pm Sunday:
National – 27,595 with 907 deaths
ACT – 114 (0)
NSW – 4425 (4)
NT – 38 (0)
QLD – 1172 (1)
SA – 502 (0)
TAS – 230 (0)
VIC – 20,346 (0)
WA – 769 (1)