The proportion of GP fees covered by Medicare has fallen to 83%, an all-time low. Neither the AMA or RACGP are surprised.
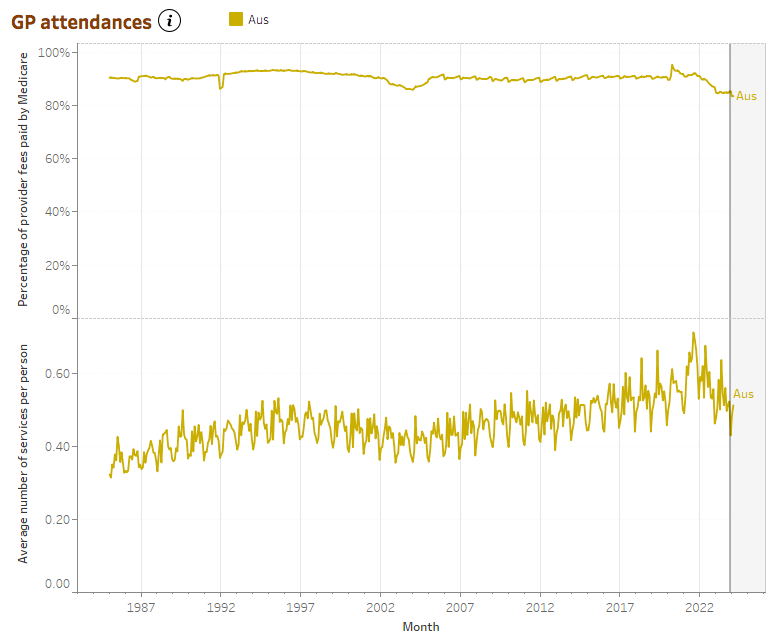
In January, the proportion of GP fees covered by Medicare hit its lowest point since the Australian Institute of Health and Welfare started presenting the data in 1985.
According to AIHW data released today, after over 15 years of relative stability at around 90% between 2005 and 2020, MBS coverage rate for GP fees now sits at around 83%.
After a spike of 95% in April 2020 at the beginning of the pandemic, coverage rates continued to follow a general downward trend throughout 2020 and 2022, fluctuating during 2021.
But after stabilising in 2023 at around 85%, the new data suggests that the decline continues into 2024, with a drop to 83.4% and 83.5% in January and February respectively, marking all-time lows.
Services per person have, however, been on the incline over the approximately 15 years until mid-2021, however this too may be on the decline.
Speaking to The Medical Republic, AMA vice president Dr Danielle McMullen said the data “reflects higher out of pocket costs, whether that is more gap fees, so less bulk billing, or higher out of pocket costs for privately billed appointments”.
Dr McMullen wasn’t surprised by the trend.
“What we’ve been hearing on the ground is obviously the cost of providing general practice, care continues to escalate,” she said.
“And the MBS rebates really haven’t kept pace for patients.
“Many practices that used to bulk bill have had to switch to mixed billing or private billing and those who already privately billed have increase their fees.
“It is still interesting to note that across the board we’re still seeing more than 80% of the cost of general practice care being borne by the government.”
RACGP President Dr Nicole Higgins agreed that the data wasn’t a “huge surprise”.
“The fact is remains that decades of neglect have made operating as a bulk billing-only GP fiscally impossible for most practices so private billing is the only option.”
Related
Dr McMullen said it would be hard to say whether the trend would persist, but it was encouraging to see that more than 80% of general practice care costs are being borne by the government.
“[The AMA] does think that measures like the tripling of the bulk billing incentive at the end of last year, did, particularly for our most vulnerable groups and in more rural and remote areas of Australia, provide that injection of funding that was needed to help people access affordable care, those who need it most.
“But there is still a lot of work to be done.”
Dr Higgins said that while the triple bulk-billing incentive was a positive step towards stemming the bleeding, and “certainly had an impact”, there remained a lot of repair needed.
Dr McMullen said she expected the strengthening Medicare and primary care reforms would help incentivise investment in general practice.
She added that the association would continue to push “to make sure that we’re rewarding those longer consultations, more complex consultations, and reducing that sort of incentive for throughput that’s really present in general practice”.
Medicare coverage of fees is also falling over time across other areas including for specialist, obstetric, anaesthetic, surgical and allied health services.
“I think it really should show government that their indexation – whether it’s general practice, other specialties, allied health – and the MBS rebates for patients haven’t kept pace with the costs of providing care.
“Across the health landscape we’re seeing even greater out of pocket costs to make sure that we keep our doors open and keep being able to deliver some care.
“But patients are paying more for it.”
Interestingly, pathology seemed to buck the trend, demonstrating general stability, if not a subtle increase, in the proportion of provider fees covered by the MBS over time.
“[Pathology] haven’t had any indexation for a long, long time.
“But they do have a huge volume of work.
“I think it’s really fundamental to our universal health care that for routine, basic pathology there is an expectation that patients won’t face large out of pocket costs.
“The pathology industry has done a good job of maintaining that and making sure that people have access to pathology services.”