The hormonal changes seem to be associated with functional decline and worsening neuronal injury.
Researchers have found an association between menopause and disease progression in MS, but were unable to comment on the potential protective effects of hormone replacement therapy.
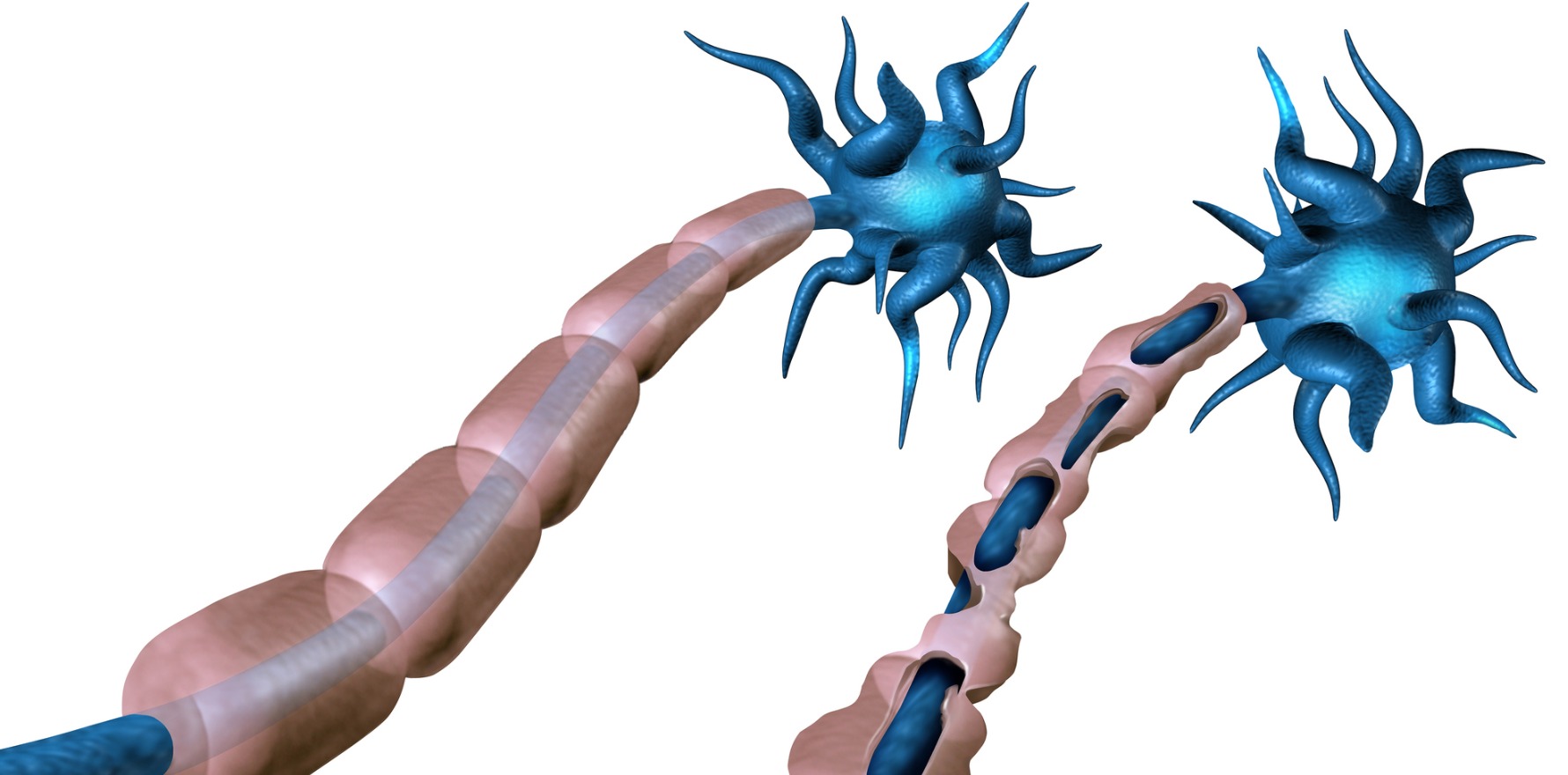
Oestrogen and other gonadal hormones are known to play a role in the immune-mediated demyelination that occurs in multiple sclerosis, which may be part of the reason why three out of four Australians diagnosed with MS are women. And while much is known about how the hormonal changes that accompany puberty and pregnancy can affect MS, the effects of menopause on symptoms and disease progression are less clear.
But a new study involving objective, prospectively collected functional and clinical measures reveals the menopause may be an inflection point in a patient’s MS journey where functional decline and neuronal injury progressively worsen. The findings were published in the journal Neurology.
“Most women are diagnosed with MS between the ages of 20 and 40 years, therefore most women with MS will undergo the menopause transition,” said Associate Professor Vilija Jokubaitis, deputy head of the Department of Neuroscience in the School of Translational Medicine at Monash University.
“Given that sex hormones modulate the immune and central nervous systems and that menopause is a time when we see a massive drop in oestradiol (the main oestrogen produced by the ovaries) and progesterone, it makes sense to explore what impact this relative loss of sex hormones might have on MS progression.”
US researchers analysed behavioural, cognitive, blood biomarker and brain imaging data from 184 postmenopausal women with MS collected as part of a series of longitudinal cohort studies with a median follow-up of 13 years. The majority of women had relapsing-remitting MS (69%) and had undergone natural menopause (85%).
At menopause, performance on the primary functional outcome measure, the MS Functional Composite (an empirical rating scale where patients are assessed on their cognitive, walking and fine motor abilities), declined – largely due to the decreases in walking-related outcomes. The longer since menopause, the greater the declines.
However, the secondary functional outcome measure, the Expanded Disability Status Scale, showed a deceleration in worsening after menopause.
Related
Professor Jokubaitis was intrigued by the contrasting results of the two functional measures.
“It could be argued that the 25-foot walk test is more sensitive to smaller changes in walking speed, as opposed to the ambulation measures in the EDSS, but I would expect these study outcomes to correlate – which they did not,” she told TMR.
Menopause was also an inflection point for the primary biomarker of the study: serum neurofilament light chain levels (a marker of axonal pathology that is associated with inflammatory activity, neurologic injury and disease progression in MS).
But MRI scans revealed there was no effect of menopause on the rate of change in total lesion volume in the brain, suggesting that neuroinflammation is not affected by the hormonal changes that occur in menopause.
These changes remained when factors such as age, disease duration, smoking status, BMI, cause of menopause and menopause hormone therapy use were accounted for in the analyses.
Professor Jokubaitis cautioned that while the results of this study indicate a decline in neurological function, the measurable impact was very small and would only be clinically discernible about 12 years after the menopausal transition. Therefore, more research is needed to better understand the impact of menopause on MS outcomes.
Only 17% of participants reported using MHT, so researchers were not able to determine whether its use provided a beneficial effect on disease and symptom progression, as suggested by previous studies in animals.
“An RCT needs to be completed to support a role for MHT as a neuroprotective add-on therapy in M0053,” Professor Jokubaitis explained.
“The trick will be to work out not only the dose/regimen of MHT as an add-on therapy, but as an add-on to which MS drug? We have many highly effective therapies available for the treatment of MS, [so] this will be a challenge.”
The selection of primary and secondary endpoints in future trials will also be critical to ensure a clinically meaningful result is achieved.
“This study indicates that future MHT RCTs should consider serum neurofilament light chain levels as a primary endpoint measure, and that T2 lesions are not likely to be informative,” Professor Jokubaitis said.
Professor Jokubaitis said women with bothersome menopause symptoms should be offered MHT, provided there were no contraindications and that this was done in consultation with their doctor.
“In the meantime, maintaining a healthy lifestyle – exercise and a good diet – are important factors that will contribute to living well with MS, and through the menopausal transition,” she said.