Children and adolescents with anxiety disorders often present initially for physical complaints, such as frequent stomach aches, writes Dr Amy Talbot
Anxiety disorders are the most common mental-health issue experienced by children and adolescents. Almost 7% of children aged four to 17 years suffer from some form of anxiety disorder across a 12-month period.
Young children (four to 11 years) are at equal risk of developing clinical anxiety as adolescents (12 to 17 years). And severity is not reduced due to their young age, with 46.2% of children and adolescents with clinical anxiety classified as having a moderate to severe anxiety disorder.1
In some ways, this is not surprising as fear is a normal part of development2 that assists young people to learn to navigate the world around them effectively and to stay safe from potential harm by facilitating avoidance of environmental threats.
Very young children may worry about being separated from their caregiver. This is in recognition that they rely heavily on their caregiver to meet their needs for survival. Adolescents may worry about not fitting in with their peers, at a time in development where peer relationships are crucial to identity formation and where cognitive development allows for the anticipation of future events.3
How then do we determine when anxiety becomes a problem?
Anxiety disorders differ from normal developmental fear on the basis of the age-appropriateness of the fear, the persistence of the fear over time, and the extent to which the fear interferes significantly with everyday functioning, such as peer and family relationships, school attendance and overall wellbeing.4
Let’s consider an example.
Tom is 10 years old. He worries about witches and ghosts and tends to avoid watching scary movies. He also worries that something bad will happen to his mother when he goes to school and has started to report stomach pains in the morning before school most days of the week for the past three weeks, occasionally leading to non-attendance at school.
Tom’s worries about witches and ghosts are a typical developmental fear for someone of his age, although they seem to be present, they do not seem to be causing significant interference (although this should be further assessed) and so may represent a typical developmental fear. Tom’s worry about harm coming to his mother, however, meets the criteria for distinguishing typical developmental worry from problematic anxiety as his fears are persisting for multiple weeks and starting to interfere with his wellbeing through reduced school attendance.
Risk factors for the development of anxiety disorders
Why might Tom have developed an anxiety disorder rather than continuing along the developmental trajectory of normative fear?
Tom may have an anxious or shy temperament, and most likely has a strong genetic vulnerability to developing an anxiety disorder, as genetics account for approximately one-third of the variance in the aetiology of anxiety disorders.5 He may also have experienced some early life or recent stressors such as family conflict, bullying, family financial stress, family separation, or life transitions (eg, moving house, changing schools, starting high school, birth of a sibling, parent return to work).
Given that greater than 80% of parents of children with anxiety disorders report significant symptoms of anxiety themselves,6 it has been hypothesised that there may also be a bi-directional learning relationship between parents and their children.
Once our fight or flight system is activated by identifying a potential threat, the natural response is to eliminate or avoid the threatening stimulus, which is highly effective for real threats to our safety but a perpetuating factor for clinical anxiety. Research suggests anxious parents teach avoidant coping strategies to their children through modelling, direct instruction about safety and harm, and reinforcement of avoidant coping behaviour, and anxious children prompt avoidant coping strategies for parents.7
Identifying anxiety disorders
Children and young people may not always have the capacity to express their anxiety in words, making behavioural observations important in determining whether anxiety might be interfering in the child or young person’s life.
Examples of behavioural indicators of anxiety in children and adolescents include:
• Frequent reports of physical health issues, such as stomach aches, headaches or sore muscles, without medical explanation
• Avoidance of age-appropriate tasks
• Refusing to attend preschool or school on a regular basis or an increase in difficulty with mobilising the child to get ready to go to school
• Difficulties with attention, concentration, organisation and/or decision making
• Increased friendship concerns, peer difficulties or withdrawal from peer group
• Sleep disturbance
• Increased irritability, tearfulness or aggression in adolescents; increased temper tantrums in younger children
• Increased clinginess or distress on separation; or withdrawal from family members
• Restlessness or increased startle response
• Noticeable decline in academic performance or increase in procrastination and inability to complete assignments on time
• Increased need for routine or increased distress at variations to routine and attempts to control others behaviour
Types of anxiety disorders
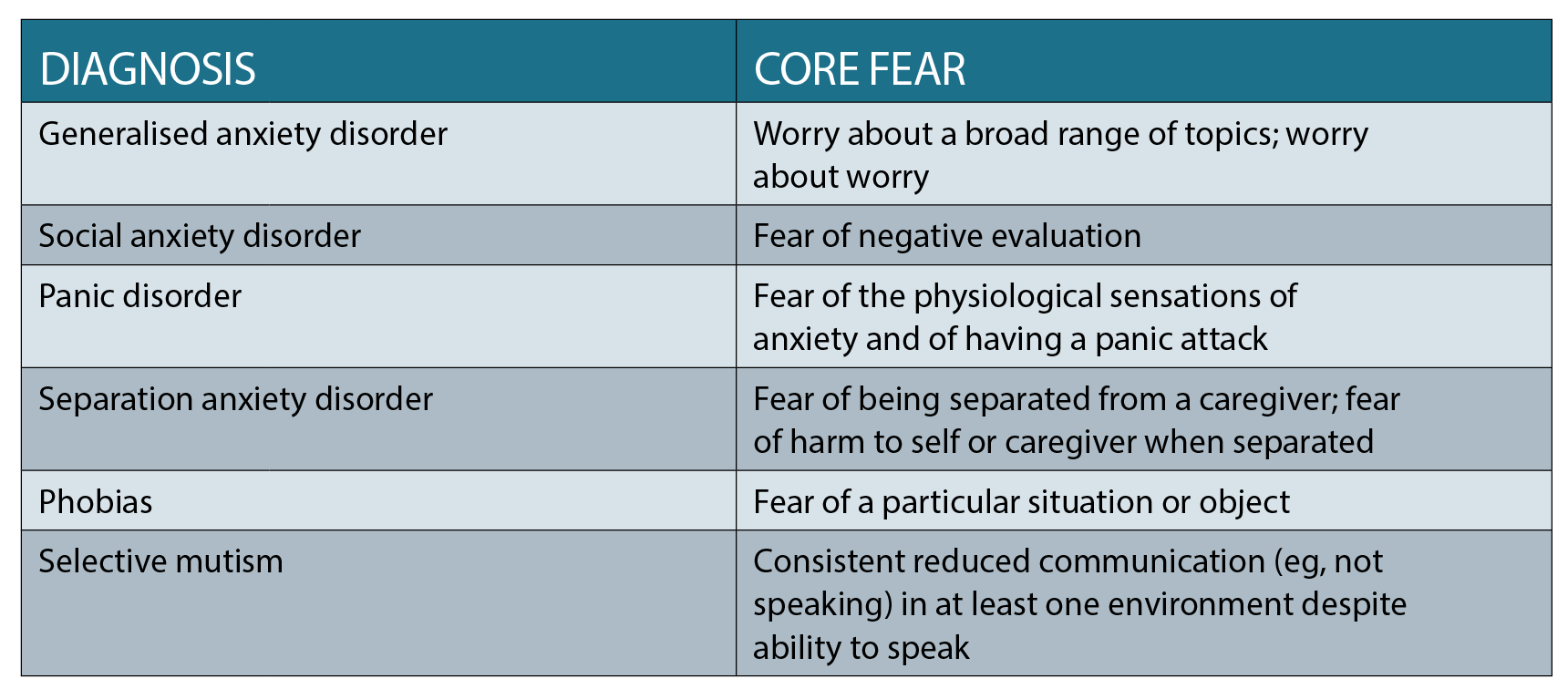
In addition to the broad behavioural indicators that a child or young person may be experiencing an anxiety disorder, young people may report more specific symptoms which can provide an indication of the type of anxiety disorder they may have. Anxiety disorders are categorised on the basis of the core fear or focus of the worry as summarised in the table on page 26.
Separation anxiety disorder and phobias are the most common among younger children (ages four to 11 years) while adolescents tend to experience a broader variety of anxiety disorder diagnoses.
Management of anxiety disorders
Anxiety disorders, by nature, significantly interfere in the daily lives of children who experience them and tend to persist long term if untreated, even into adulthood, due to the perpetuating nature of avoidant coping responses.8 Anxiety disorders in childhood are also risk factors for the development of other mental-health difficulties in adolescence and adulthood.
Although fear is a normative part of child development, when fear starts to interfere with relationships, school or other life domains, or persists for more than a few weeks, early identification and management is essential. This is especially the case for children of anxious parents or parents with a history of anxiety disorders themselves, given the strong combined impact of genetics and reinforcement of avoidant coping strategies on the development of clinical anxiety in children.
Cognitive Behavioural Therapy (CBT) has consistently been shown to be beneficial in the management of childhood and adolescent anxiety across the various diagnostic categories, with demonstrated long-term improvement in symptomatology.9,10
CBT is likely to involve education for the young person and the family about the physiological aspects of anxiety and the relationship between thoughts, feelings and behaviour, as well as teaching skills to challenge unhelpful thinking styles and reduce avoidant coping responses. Ideally interventions will involve a full family approach to support the development of a consistent environment within which non-avoidant coping responses are encouraged and reinforced.
From a medical management perspective, as children and adolescents often present initially for physical complaints (such as frequent stomach aches) as opposed to anxiety, a thorough medical assessment may be required in order to confirm the diagnosis and appropriate referral options.
For mild to moderate presentations of anxiety in child and adolescent populations, the RANZCP guidelines indicate that CBT should be used as the primary intervention, while deferring use of pharmacotherapy.11 Where children and adolescents present with more severe functional impairment SSRIs may be beneficial in addition to CBT. Where medication in addition to CBT may be indicated; close monitoring and review, with slow increase in dosage and consultation from a paediatrician or child and adolescent psychiatrist is recommended, as is a thorough discussion with the family regarding possible side effects and how to manage any increases in safety concern. 9-11
Guidance on supporting anxious students during competitive exams
Young people with anxiety disorders are particularly vulnerable during competitive examinations and other situations where they are likely to be evaluated, particularly those with social anxiety disorder.
In considering the normative fear model, it is important to note that it is normal to feel some level of anxiety leading into examinations, and that this anxiety is likely to promote adaptive behaviours such as studying effectively.
Just like with other situations, anxiety becomes problematic when it starts to interfere in the young person’s ability to engage with their life effectively. In exam situations this could include such high anxiety that information cannot be retained due to poor concentration and subsequent memory difficulties, difficulty making decisions with regard to selecting appropriate information to review, procrastinating with study or skipping exams altogether.
When supporting young people through competitive examinations it is important to provide consistent feedback that their worth is not determined by their performance in an examination, to assist them to focus on their behaviour (eg, study) rather than on outcomes (eg, marks) and to assist them to use factual information to challenge any catastrophic thinking about the outcomes of the examinations.
Young people should be provided with as much information as possible on the different pathways into study post school to avoid getting caught up in black and white thinking, and should be encouraged to maintain a balanced focus on interests outside of academic tasks.
In most circumstances, signs of clinical anxiety will be present prior to the occurrence of competitive examinations.
The best way to support young people with anxiety is to identify the signs early and to refer them for CBT intervention prior to the commencement of examinations to allow time for the young person to develop additional skills that will enable better coping when the examinations do occur.
All interventions, both psychological and medical, require time to be effective. The most useful way to support young people is to identify their symptoms early enough that they have time to develop effective non-avoidant coping skills prior to being required to engage in stressful and anxiety provoking situations.
Dr Amy Talbot is a clinical psychologist and director of The Talbot Centre in Northwest Sydney, a clinic with a strong focus on supporting families to effectively navigate the difficult tasks of growing up
References
1. Department of Health. The Mental Health of Children and Adolescents. Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. [Internet]. 2015. [cited 2017 December 1]. Available from https://www.health.gov.au/internet/main/publishing.nsf/Content/9DA8CA21306FE6EDCA257E2700016945/%24File/child2.pdf
2. King NJ, Hamilton DI, Ollendick TH. Children’s phobias: A behavioural perspective. Chichester, UK: John Wiley & Sons; 1988.
3. Gullone E. The development of normal fear: A century of research. Clin Psych Rev. 2000; 20(4):429-451.
4. Miller LC, Barrett CL, Hampe E. Phobias of childhood in a prescientific era. In A. Davids (Ed.), Child personality and psychopathology: Current topics. (Vol. 1, pp. 89–134). New York: John Wiley & Sons; 1974.
5. Eley TC. Contributions of behavioral genetics research: Quantifying genetic, shared environmental and nonshared environmental influences. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 45– 59). New York: Oxford University Press; 2001.
6. Ginsburg GS, Schlossberg MC. Family-based treatment of childhood anxiety disorders. Int Rev Psychiatry. 2002; 14:143–154.
7. Fisak B, Grills-Taquechel AE. Parental modelling, reinforcement and information transfer: Risk factors in the development of child anxiety? Clin Child Fam Psychol Rev 2007 Sept;10(3):213-231.
8. Bernstein GA. Borchardt CM, Perwien AR. Anxiety disorders in children and adolescents: A review of the past 10 years. J Am Acad Child Adoles Psychiatry. 1996; 35:1110–1119.
9. Wang Z, Whiteside SPH, Sim L, Farah W, Morrow AS, Alsawas M, et al. Comparative effectiveness and safety of cognitive behavioural therapy and pharmacotherapy for childhood anxiety disorders: A systematic review and meta-analysis. JAMA Pediatr. 2017 Nov 1;171(11):1049-1056.
10. Kodish I, Rockhill C, Varley C. Pharmacological aspects: Pharmacotherapy for anxiety disorders in children and adolescents. Dialogues Clin Neurosci. 2011;13:439-452.
11. RANZCP. Clinical guidance on the use of antidepressant medications in children and adolescents. [Internet] March 2005. [cited 2017 December 1] Available from https://www.ranzcp.org/Files/Resources/College_Statements/Practice_Guidelines/Clinical_Guidance_on_the_use_of_Antidepressant_med.aspx