Chronic autoimmune neuropathies are extremely heterogenous disorders with varied clinical presentations, prognoses and responses to therapy
Neuropathy and neuromuscular disorders affect millions worldwide. The immune-mediated neuropathies are caused by an aberrant immune response to components of the peripheral nerve and may produce severe weakness and disability.1
The chronic forms include chronic inflammatory demyelinating polyneuropathy (CIDP) and multifocal motor neuropathy (MMN).
CIDP is the most common treatable neuropathy in the western world and typically presents with weakness and sensory impairment. Patients experience recurrent relapses or a progressive course requiring long-term treatment.1
MMN is a related disorder which affects peripheral motor nerves leading to weakness and muscle wasting and is typically responsive to immunomodulatory treatment.2
In contrast, degenerative motor neuropathies (e.g, motor neuron disease) cause progressive weakness and disability without an effective treatment and may be difficult to differentiate from the treatable immune-mediated neuropathies.3
The chronic autoimmune neuropathies frequently result in significant functional disability, including difficulty with walking and ability to carry out self-care and activities of daily living.
Hence, both CIDP and MMN are costly in terms of burden on patients. In addition, they require long-term costly treatments causing a tremendous burden on healthcare systems.
Immunomodulatory treatments such as intravenous immunoglobulin (IVIg; containing pooled immunoglobulins from the plasma of blood donors), remain the most successful in treating acquired immune-mediated neuropathies.
In 2015-16, a total of 4.98 million grams of IVIg was issued in Australia, representing a cost of $544.6 million. Neurology remains the discipline using the greatest amount of IVIg with CIDP being the most frequent indication for IVIg use within neurology.4
The chronic autoimmune neuropathies, however, are extremely heterogenous disorders with varied clinical presentations, prognosis and response to therapy.
Extraordinarily for such an expensive therapy, a “trial and error” approach is used as we still do not know which patients will benefit from IVIg treatment. While some patients will respond to first-line therapy with standard doses of IVIg, others will require higher doses, and some may not respond at all but respond to alternative treatments such as steroids or plasma exchange.
Unfortunately, little is known about disease mechanisms, limiting targeted treatment approaches.
Neurophysiology is the major tool used in the diagnosis and classification of neuropathy. Nerve conduction studies allow for assessment of the amplitude of responses as well as conduction velocities.
Supplementary investigations which may be performed, include examination of cerebrospinal fluid, imaging and immunological assays. Despite these tools, establishing a diagnosis can still be difficult.
Two major areas of research interest lie in the identification of antigenic targets and advanced imaging techniques. These are:
Antigenic targets and autoantibodies in inflammatory neuropathy
Although antigenic targets and disease pathophysiology of chronic immune-mediated neuropathies remain largely undefined, the recent discovery of IgG4 antibodies directed towards neurofascin-155 (NF155), neurofascin-186 (NF186) and contactin-1 (CNTN1), protein components found on peripheral nerves, has been a major advance in the area of chronic autoimmune peripheral nerve disorders.
Patients with IgG4 antibodies against one of these proteins have distinct clinical phenotypes. The NF155 IgG4 phenotype is characterised by a younger age of onset, predominantly distal neuropathy and disabling tremor.5,6
In contrast, anti-CNTN1 IgG4 neuropathy is typically characterised by older age, aggressive onset, motor predominance, and early axonal damage.7 Although these antibodies are only found in 5 to 10% of patients with CIDP, they are of critical importance due to important treatment and prognostic implications.
Patients tend to be refractory to IVIg but may respond to corticosteroids or other immunosuppressants. Rituximab has proven effective in patients who are refractory to IVIg and corticosteroids6 but is an expensive treatment with significant adverse risks.
To-date, there are no clear guidelines on the best first-line treatment to minimise the risk of permanent axonal loss and disability while minimising adverse effects.
Furthermore, in the remaining 90 to 95% of patients with CIDP, no antibody is detected, and the antigenic target remains unknown.
This is currently an area of great research interest.
Neuroimaging as a diagnostic tool
A practical challenge faced by clinicians is the differentiation of inflammatory neuropathies from degenerative neuropathies, a critical distinction due to the treatable nature of the immune-mediated neuropathies.
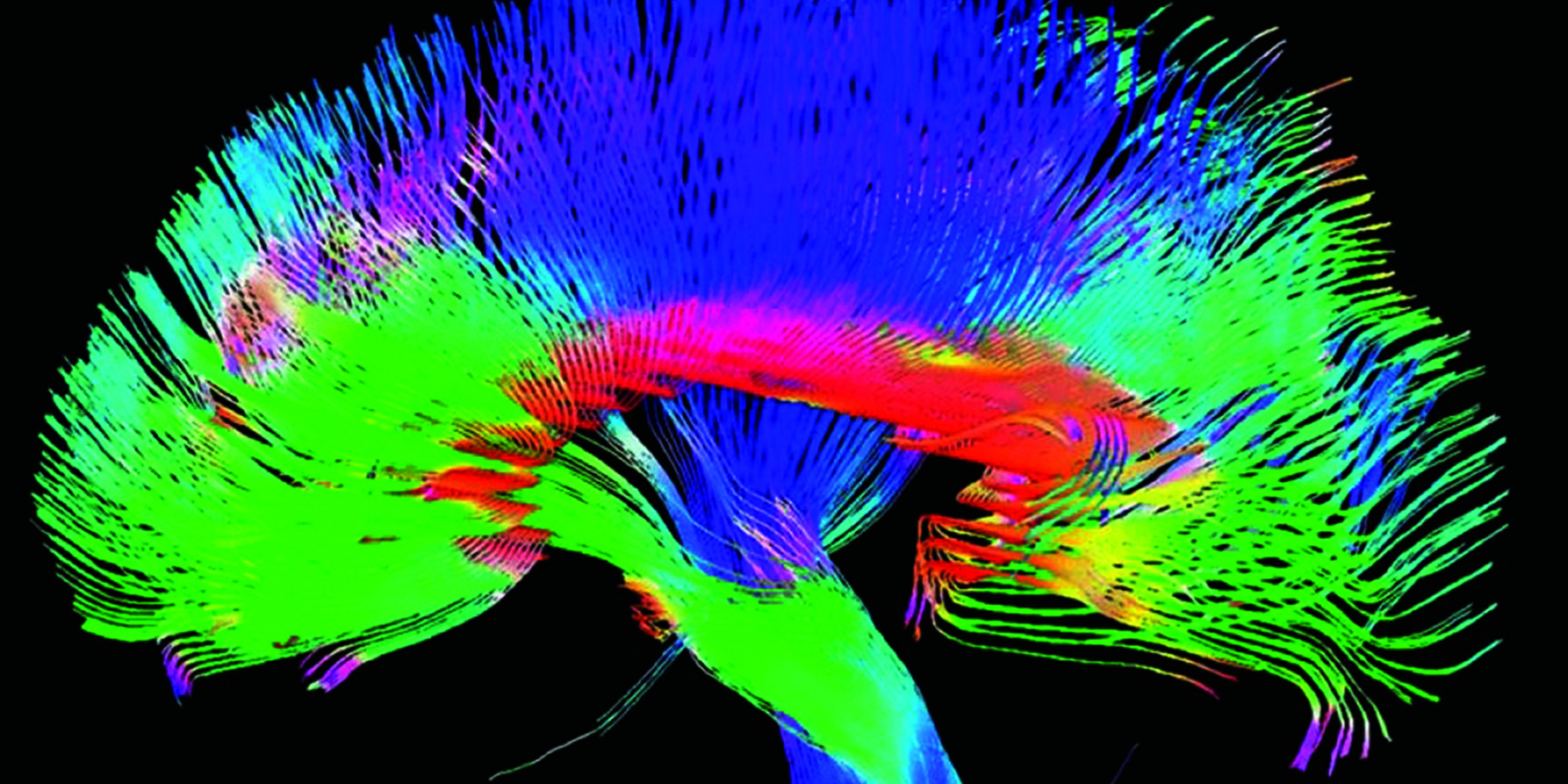
Novel magnetic resonance imaging (MRI) techniques, including MR neurography and diffusion tensor imaging (DTI) have recently emerged as useful tools in assessing peripheral nerve structure allowing for greater insight into nerve pathology, and with further research are likely to prove valuable as diagnostic tools.9
While conventional MRI provides poor visualisation of peripheral nerves, MR neurography allows for assessment of nerve morphological structure.
In contrast, the principle of DTI is based on the diffusion of water molecules with the technique being highly sensitive to subtle changes in tissue microstructure.9
Both techniques have shown promise in immune-mediated neuropathies. MR neurography can differentiate typical CIDP, in which nerve enlargement is symmetrical and maximal at the nerve roots from multifocal acquired demyelinating sensory and motor neuropathy (an atypical variant of CIDP), in which nerve enlargement is typically asymmetrical and multifocal.10
Alterations in diffusion parameters in MMN have allowed for greater insights into disease pathogenesis demonstrating that both myelin and axonal dysfunction are prominent in MMN.11
What are the major struggles in clinical practice?
From a clinical perspective, the major challenges faced by neurologists are:
• Diagnostic difficulties: chronic autoimmune neuropathies can be difficult to distinguish from neuropathies without effective treatments (such as motor neuron disease or hereditary neuropathies) and often costly treatment trials of immunomodulatory therapy, such as IVIg, are instituted.
• Early institution of the most appropriate therapy: response to first-line treatment with IVIg is extremely variable between patients and a “trial and error” approach is used often resulting in a delay in the institution of effective immunotherapy.
How will our research address these struggles?
Our research will address these issues by utilising a number of tools to answer the following questions:
• What are the specific clinical and neurophysiological features that will allow us to determine what treatments will be most effective for a given patient with immune-mediated neuropathy?
• How can we use novel imaging techniques as diagnostic tools in autoimmune neuropathy and in the differentiation from disease mimics?
• How can the clinical severity, nerve conduction study results and antibody levels be used to determine the most effective and safest treatment in patients with CIDP associated with the recently discovered anti-neurofascin-155 or anti-contactin 1 IgG4 antibodies, and;
• What other antigenic targets and autoantibodies are associated with CIDP and MMN and how do they correlate with clinical phenotypes and treatment response?
By answering these questions, we hope that the diagnosis and management of patients with chronic autoimmune neuropathies will be significantly improved.
Dr Nidhi Garg is a neurologist currently completing her PhD at the Brain and Mind Centre at The University of Sydney.
The team for the Brain Foundation Grant consists of Dr Garg, Dr Susanna Park, Dr Emily Mathey, Professor Michael Barnett and Professor John Pollard
References:
1. Mathey EK, Park SB, Hughes RA, Pollard JD, Armati PJ, Barnett MH, et al. Chronic inflammatory demyelinating polyradiculoneuropathy: from pathology to phenotype. J Neurol Neurosurg Psychiatry. 2015;86(9):973-85.
2. Vlam L, van der Pol WL, Cats EA, Straver DC, Piepers S, Franssen H, et al. Multifocal motor neuropathy: diagnosis, pathogenesis and treatment strategies. Nat Rev Neurol. 2011;8:48-58.
3. Garg N, Park SB, Vucic S, Yiannikas C, Spies J, Howells J, et al. Differentiating lower motor neuron syndromes. J Neurol Neurosurg Psychiatry. 2017a;88(6):474-83.