New research forecasts dire straits unless voluntary-assisted dying is financially supported.
Remuneration for voluntary assisted dying (VAD) has come into question, with new statistics showing that practitioners are receiving inadequate compensation for the care.
Voluntary Assisted Dying Australia and New Zealand (VADANZ) is an advocacy body for VAD practitioners.
According to its 2025 survey, nearly two thirds (63%) of VAD practitioners felt they were unfairly remunerated and over a quarter (27%) of practitioners reported that they provided unpaid VAD care.
VAD has long foregone its taboo past in healthcare, with the practice legal in every Australian jurisdiction bar the Northern Territory, which is expected to pass legislation soon.
Per the survey, the current state of healthcare has not yet adjusted to properly support the form of care, with only one third of practitioners having received any state government reimbursement.
Respondents also reported widespread dissatisfaction with state government support, with only New South Wales reporting a slim majority (51%) of remuneration satisfaction.
“All Australian jurisdictions, apart from the Northern Territory, have taken the courageous step of legalising VAD,” VADANZ president Dr Andrea Bendrups said.
“Person-centred services have been established in all these jurisdictions which are delivering high quality end-of-life care, but relying on clinical altruism to do so.
“We urgently need to ensure those who provide this care have the support they need to continue doing so.”
There are no dedicated Medicare items for VAD, leaving practitioners uncompensated for associated non-clinical work.
Currently, the MBS excludes “euthanasia and any service directly related to the procedure.”
“However, services rendered for counselling/assessment about euthanasia will attract benefits,” the MBS page reads.
This has put practitioners in the position of privately charging for VAD services.
VADANZ is calling for several reforms to address this issue focusing on clear guidance for billing and dedicated MBS items to fairly compensate practitioners such as:
- Dedicated MBS items recognising the unique demands of VAD care.
- Comprehensive fee schedules covering all aspects of care, including travel.
- Increased numbers of funded hospital roles to provide stability for practitioners.
- Clear state guidance on billing options to reduce uncertainty.
- Federal updates to MBS Explanatory Notes to remove outdated restrictions on VAD items.”
VADANZ has also suggested implementing a model similar to New Zealand, with “structured fee‑for‑service payments across five modules, additional remuneration for complex cases, and travel allowances.”
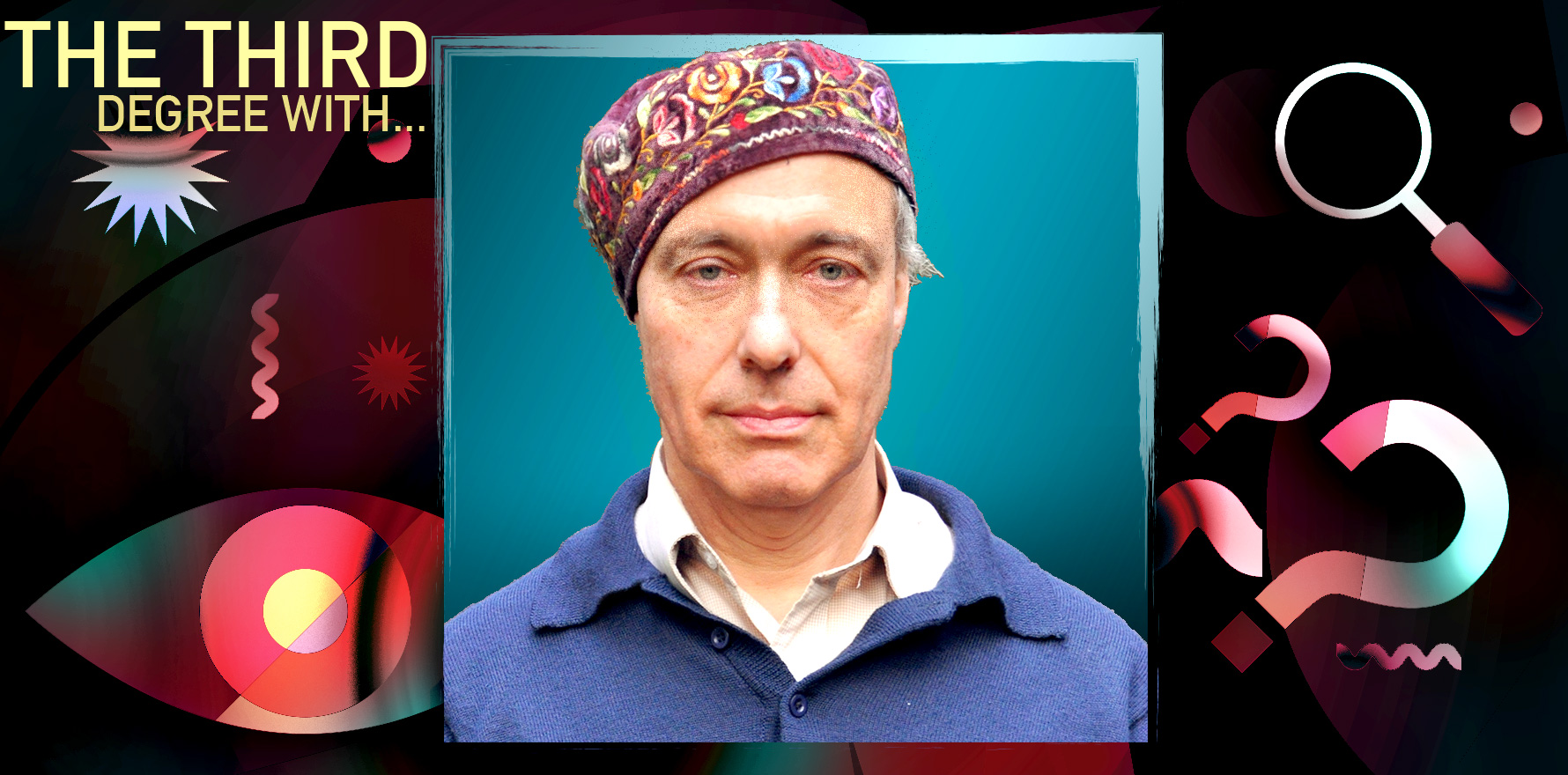
“In order to create a Medicare item number, there would need to be a degree of political consensus at the federal level, and that has proved difficult to achieve,” assisted dying researcher and philosopher Professor Paul Komesaroff told The Medical Republic.
Related
“I would court attempts to encourage the federal health minister to seek to achieve a degree of consensus at the federal level to withdraw that provision in the Crimes Act and to establish one or more Medicare item numbers.
“It’s clearly out of step with the way in which the Australian community has chosen to see voluntary assisted dying as an appropriate service that has a well-established place in clinical care.”