Workforce retention and burnout are still big problems among general practices in the Hunter, New England and Central Coast.
Financial stability, strategic planning and morale are improving in general practices in the Hunter, New England, and Central Coast regions, but workforce shortages remain a critical issue, according to a new report.
The latest update from the Sustainability and Viability Initiative in the Hunter New England and Central Coast (HNECC) Primary Health Network shows that just 36% of practices showed signs of financial instability in 2025, an improvement from 49% in 2024.
SAVI was launched early in 2024 to tackle concerns around the financial, operational and workforce sustainability of general practices in the HNECC PHN. It is an initiative of the HNECC, and other PHNs are looking to adopt a similar initiative, a spokesperson said.
This article originally ran on TMR’s sister site, Health Services Daily. TMR readers can sign up for a discounted subscription.
The latest report is based on responses – mainly from practice managers – from 189 practices that also completed a check-in survey in 2025.
The report found that the proportion of practices uses strategic planning tools rose from 22% in 2024 to 74% in 2025.
But 69% of practices reported relying on WIP and PIP incentives as core income – still an improvement on 85% in 2024 – and only 6.9% of practices did not rely on those streams.
One third of practices said they have difficulty keeping up with bills and 16% said they couldn’t afford to replace essential equipment such as vaccine fridges.
“We face enormous expenses, with little incoming revenue and no profit,” one respondent told researchers.
“Doctors often leave early due to low income because the practice cannot afford to pay them more.”
The report said financial sustainability remained a central concern for general practices across the region.
“Despite efforts to optimise income through MBS billing and incentive programs, many practices continue to face financial stress, unstable cash flow, and limited capacity to invest in essential resources,” the report said.
“Survey data reveals a heavy reliance on external funding streams such as WIP and PIP, with service-generated income often insufficient to maintain viability.
“These pressures highlight the need for improved financial literacy, strategic planning, and targeted support to ensure long-term business resilience.”
Overall, workforce morale rose from 41% to 58% in the same period.
“Practices investing in staff wellbeing and team cohesion report improved morale and retention,” the report said.
But workforce shortages were still a critical issue, with 55% of practices reporting that attracting and retaining staff was a major barrier.
“GPs are leaving the workforce due to retirement, parental leave, family commitments, disillusionment, and burnout from increased demands on their time,” one respondent said.
The report said high turnover and burnout impact continuity of care and team cohesion.
“Survey responses reveal widespread shortages of GPs and nurses, high turnover, and difficulty recruiting experienced staff,” the report said.
“These issues strain daily operations, reduce morale, and disrupt continuity of care.”
The top workforce issues in 2025 were clinical staff shortages, high turnover and leave, limited practice manager capability, resistance to change and training gaps, and weak leadership and support systems.
While 34% of practices said they would experience disruption to care and income if a nurse took unplanned leave, that percentage is an improvement on 40% in 2024, “suggested improved staff resilience”, the report said.
Practices also reported high administrative burdens, especially from phone calls and
compliance requirements, as well as limited adoption of technology and a lack of integrated systems.
“The quantity of phone calls, predominantly from elderly patients, drains our admin team,” one respondent said.
Related
“I do not know how to address this issue.”
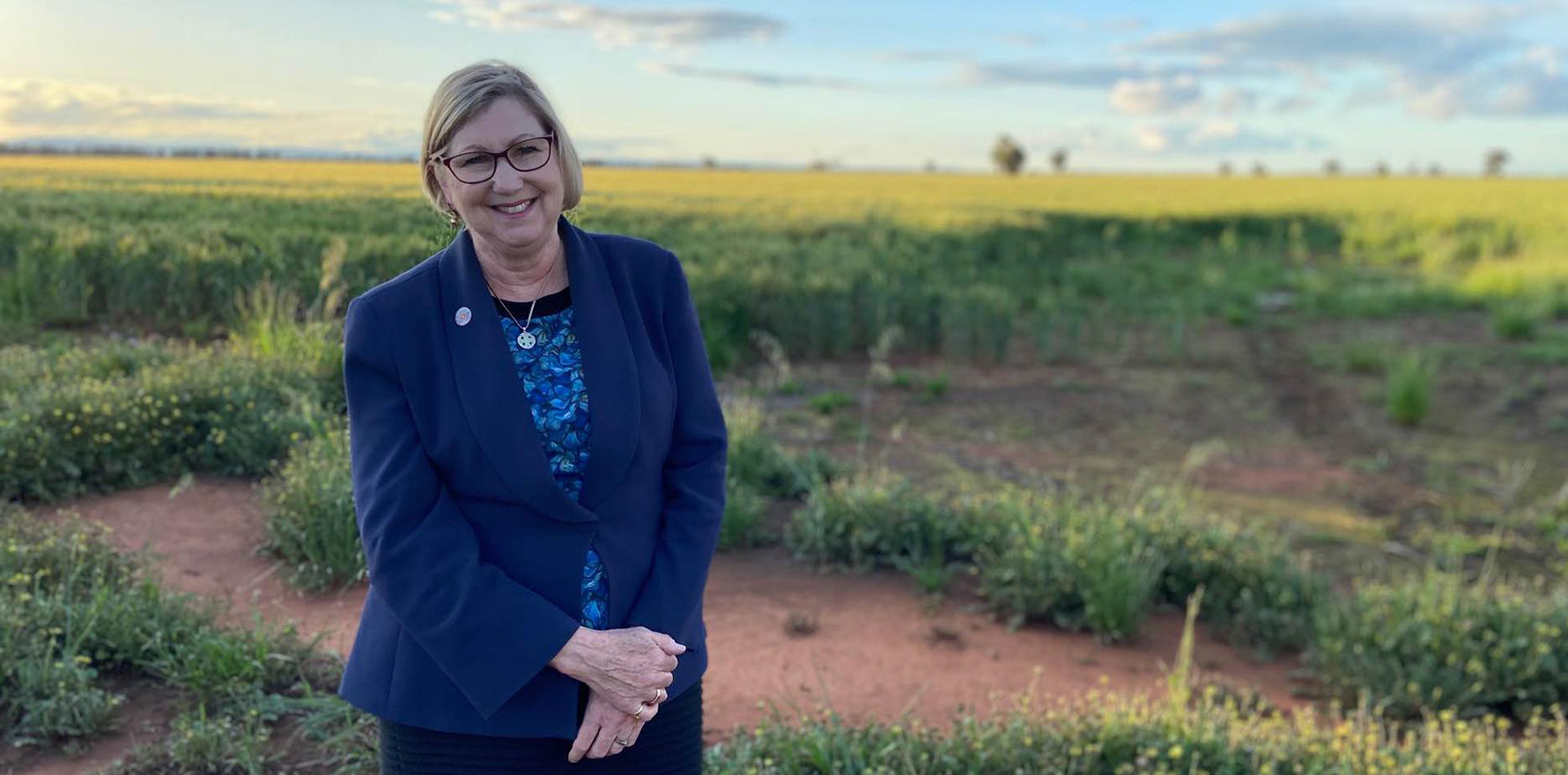
Dr Alison Koschel, executive manager of primary care workforce and access at HNECC PHN, said the latest report showed that progress had been made and engagement in the program was strong, but general practices still faced significant challenges.
“SAVI’s tailored, data-driven approach is helping practices build resilience, improve performance, and sustain viability,” she said.
“Continued investment in workforce, operations, and financial support will be essential to ensure equitable access to primary care across the Hunter New England Central Coast region.”
Dr Koschel said workforce retention was a critical challenge for practices.
“Addressing this requires targeted strategies such as reducing administrative burden, improving workplace support systems, and creating pathways for professional development for those in key roles.
“While some solutions may involve broader advocacy for general practitioners, these findings underscore the need for PHN to support workforce initiatives, as workforce capacity is the foundation for all other improvements in general practice.”
Read the full General Practice Viability Insights Report here.