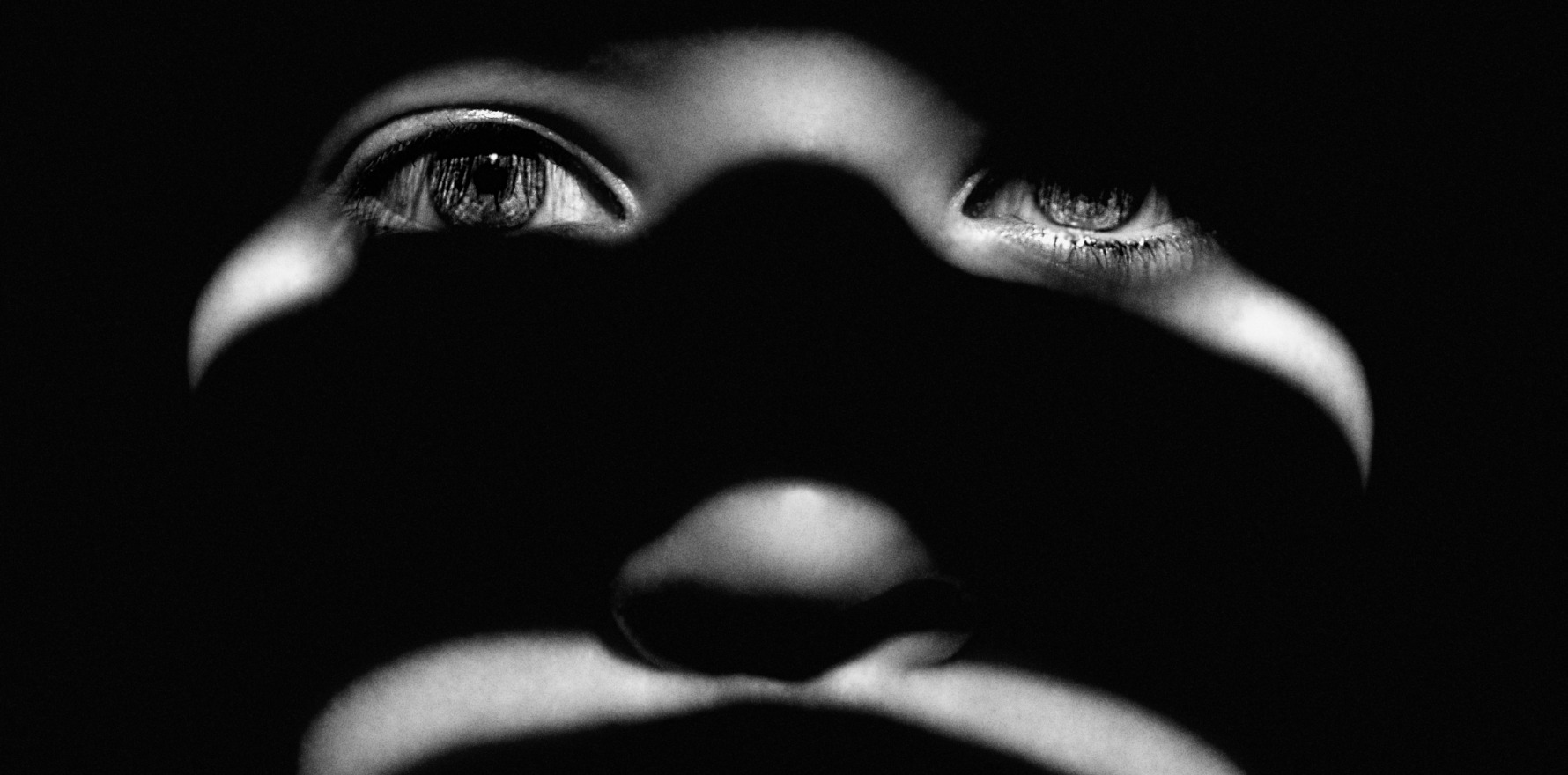
Domestic or intimate partner violence is as common as asthma or diabetes, yet it often still flies under the radar.
Changing practice culture can go a long way toward identifying patients who may be experiencing or at risk of experiencing domestic violence, according to one GP expert.
Professor Kelsey Hegarty, a researcher and GP who heads up the University of Melbourne’s Safer Families Centre of Research Excellence, said current undergraduate and postgraduate medical training programs often failed to spend a meaningful amount of time on domestic violence education.
“[Before getting into this area of work], I was doing a lot of mental health work and reading in the newspaper about one in four women having experienced domestic violence – and that was 25 years ago,” she told The Medical Republic.
“[I remember] thinking, ‘I haven’t seen anybody’, but I also wasn’t asking. That’s what started to get me motivated.
“And once I started to recognise that this is as common a problem as asthma or diabetes – and how much training we have on those chronic illnesses, [compared to] hardly anything on this – it became my passion.”
The Safer Families Centre was recently commissioned by Tasmania’s Primary Health Network (PHN) to deliver a fully funded workshop for GPs working in the island state.
Part of Professor Hegarty’s workshop involves training non-clinical practice staff to recognise potential signs that a patient is experiencing domestic abuse.
“For the reception staff, we talk about what they might notice in the waiting room … sometimes interactions between partners might happen where they notice something that they can then talk to the practice manager about that, or they might notice that a partner is ringing up all the time and trying to get information about a patient,” Professor Hegarty said.
“We … are really trying to change the culture to be where everybody has a role.”
The other part to this approach is treating domestic violence similarly to any other chronic health issue by putting up posters and notices in the clinic waiting room.
“Research shows that GPs are the highest professional group disclosed to by current survivors,” acting PHN CEO Susan Powell said.
“Of those who disclose, approximately one in three survivors experiencing current partner violence (and one in four survivors who have experienced past partner violence) seek help from GPs.
“At least one in 10 women attending general practice will have experienced family violence, which for a full-time GP translates to around five women per week.”
Professor Hegarty said that while GPs may see five women per week who have or will one day have experienced domestic violence, not all of them are necessarily identified.
“What we try and do is overcome some of the barriers [to that identification] on the practitioners’ side,” she said.
Related
“One of them is that GPs don’t have a lot of training in their undergraduate degrees or their postgraduate degrees [about domestic violence].
“So for them, it’s often a very new thing to be thinking about how to ask [their patients], and what we do is provide scripts for how to introduce the topic.”
These include non-labelling questions like whether the patient is afraid of their partner, whether they have felt controlled and whether they are being constantly put down by their partner or a family member.
“Part of our program is just giving GPs and primary care nurses and Aboriginal Health Workers the words to say,” Professor Hegarty said.
“They’ve got the skills from other areas. They just haven’t been taught the scripts.”