While pes anserine bursitis is a common finding in adults, its presence in a child should be investigated
A 10-year-old girl presented with painful swelling over the medial side of her knee, with recent exacerbation, and occasional knee locking. There was no history of recent trauma. The patient was constitutionally well. On examination, there was fluctuant, painful swelling in the proximal anteromedial lower leg, just below the joint line.
She was referred for a radiograph and MRI for further investigation.
On radiographs, there is a bony exostosis in the medial proximal tibial metaphysis, pedunculated in nature and pointing distally away from the knee joint. This is not associated with bony destruction, periosteal reaction or pathological fracture. There is, however, the impression of a soft tissue mass that is potentially concerning.
MRI shows the presence of a pedunculated osteochondroma, with the cortical continuation of the lesion contiguous with the tibia. There is no associated marrow oedema, fracture or soft tissue mass. The cartilage cap on the osteochondroma is minimal. The fluctuant soft tissue swelling is in fact due to prominent fluid in the pes bursa situated immediately adjacent to the osteochondroma. This would indicate local irritation of the bursa and bursitis.
Osteochondromas are benign bony lesions that can be complicated by pressure effects such as neurovascular compromise, adventitial bursitis (due to friction of adjacent soft tissues), traumatic fracture and sarcomatous transformation.
Pain and soft tissue swelling without a history of trauma can herald malignant transformation which can be characterised by a thick soft tissue cap, soft tissue neoplastic mass, bony destruction or pathological fracture. However, painful atraumatic swelling can also be caused by bursitis, as in this case.
A combination of radiographs (to assess bony destruction, periosteal reaction or pathological fracture) and MRI (to assess whether soft tissue swelling is due to bursitis or neoplastic tissue) helps to differentiate these two conditions.
Management for osteochondromas would include assessment of whether there are multiple osteochondromata in the body (a condition called “diaphyseal aclasis”, which is hereditary) or family history, as this would increase the risk of sarcomatous transformation. Although they can be managed conservatively, the location of this lesion would likely result in recurrent symptoms and operative resection would be relatively straightforward.
Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He works in Sydney at St Vincent’s Private Hospital and Mater Hospital.
Figure A: Knee radiograph showing a bony exostosis (blue arrow) arising from the proximal medial tibial metaphysis, pointing distally. There is surrounding soft tissue swelling (red arrow) but no fracture or bony destruction.
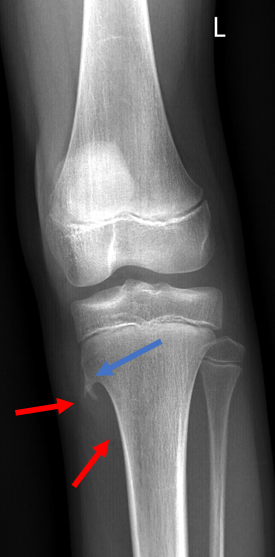
Figure B: Coronal PD and T2 fat saturated images showing the osteochondroma with a thin cartilage cap (blue arrow) and fluid in the adjacent pes bursa (red arrow). There is no soft tissue solid mass or marrow oedema.
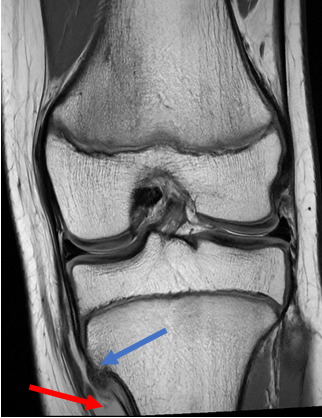

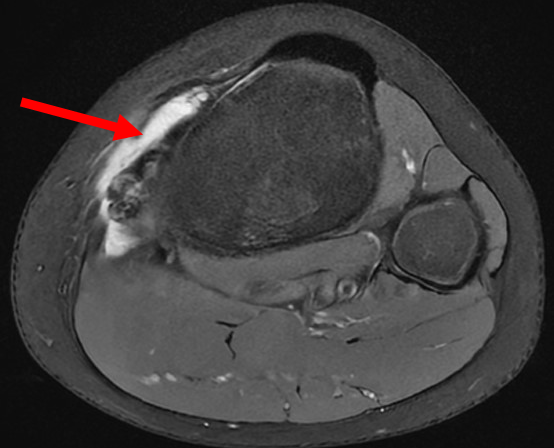
Figure C: Axial T2 fat saturated image showing a prominent fluid filled pes bursa.