There’s more change coming the way of GPs than ever in the history of the profession. No one likes change, but as the saying goes, things don’t change, we do.
Who Moved My Cheese is one of my favourites of the potboiler management books of the late 1990s. Like all those books I mostly just read the dustcover.
The ground-breaking (not) idea in this one is change and people don’t go together very well.
Hmmm … nearly all these management books somehow turn out pages and pages on one very simple and obvious thing with supposed breakthrough ways of dealing with that thing. But how about this dustcover promise from Who Moved My Cheese if you’re a GP these days:
You’ll learn how to anticipate, adapt to and enjoy change and be ready to change quickly whenever you need to.
You won’t.
It’s just not the human condition. Add healthcare and medicine to the mix and you’re really in trouble when you want to effect or adapt to change.
This is especially so for the profession of general practice given just how much change is coming its way.
We held the Wild Health One Healthcare System Summit (videos of sessions coming) in Canberra this week, and over one and half days a lot of people got to reflect on just how much change the federal government is contemplating for the entire healthcare system, with GPs at the epicentre of change.
It’s a lot … maybe even too much.
It’s comforting for me that you really do get the feeling that somewhere deep in the bowels of the Department of Health, Disability and Ageing, there’s a room with a giant whiteboard and every moving part of the healthcare system – even those myriad of things that interact with it on the edges but perturb it – is on it.
And that, regularly, certain groups go down there with their whiteboard rubber and marker pens to update and redo parts of the master plan with new information they’ve learned. There’s lots of crossing squiggly lines, arrows and shapes, question marks and comments.
DoHDA people deny the existence of the room and the whiteboard, if you’re wondering. But it’s there, even if metaphorically.
DoHDA has quite a lot of understanding and intent and is doing a ton of planning around that intent (maybe all those reviews had some effect after all), and now they have a six- year runway (probably).
Without having to read Who Moved My Cheese, a simple message for general practice might be, “strap yourselves in, and keep an open mind”.
The narrative of GPs being the pivot point for system transformation around ageing and chronic care has, until now, been mostly just that – a narrative: story-telling that makes people feel good, often spouted by senior politicians, at both the state and federal level to calm everyone down, while they kick that reform can just a little further down the road.
So far not much has happened. In fact, the funding for general practice has actually gone backwards by a few percent in the last few years, while funding for hospitals has gone up – which sort of confirms nothing much has happened yet.
But things are starting to move.
There are eight things in play or soon to be in play, given initiatives being planned and private sector dynamics, that might actually set the profession on an actual path to the “GPs are the hub of system reform” narrative.
Here are the first four, with four to come next week, so don’t worry too much if you’re struggling by No 3.
1. 60/40, MBS rationalisation and other adventures in funding reform
If you’ve been living under a rock you won’t have heard that the fine folk running Medicare want to shift the funding emphasis for GPs from 90% fee-for-service to 60% fee-for-service and 40% “blended” funding.
If you’re a GP hearing this for the first time the acronym for fee for service – FFS – might resonate.
FFS because GPs hear lots of horror stories about the UK’s NHS and “capitation”, probably because we seem to have most of the UK GP sector working for us now, most of them seeing themselves as refugees from a system that pretty much melted down, thanks to how the UK government managed that funding model.
There are a couple of things to keep in mind about this change – which I’m going to say is coming whether you like it not, so it’s probably best to try to figure out how to make it work for you rather than simply resist it (remember, things don’t change, you do):
- The changes are not going to be Big Bang – they are going to be iterative and there’s going to be consultation and co-design. In the case of the My Health Record same-day patient information rule on mandatory uploads, which looked horrific initially to GPs because of patient communication on delicate matters, the government listened and adjusted to take account of GPs concerns … a good start and how the government views the process; and,
- You can’t effect change to dovetail how GPs work with hospitals, aged care and disability, unless you get targeted on some things around outcomes somehow, and this is what blended funding can do. It can be tactical and targeted. One-size-fits-all funding models don’t suit where healthcare is going in Australia. We see this most starkly in how healthcare works in rural and remote versus the city. We need flexibility, and blended funding does offer that opportunity. It also needs collaboration and constructive input for the profession but the government wants that.
There’s a lot more on 60/40 but there’s also a lot more funding reform to mention so we have to stop there for now.
Three hundred and fifty MBS items for GPs is too many and creates a fair bit of system inefficiency.
Related
The government is going to rationalise this number and by quite a lot. They aren’t going down to 20 (which is what someone joked about this week at the One Healthcare System Summit) but it’s not going to be 320 either – maybe somewhere between 120 and 220 (I’m guessing).
That’s a very big change that will need the same collaboration and co-design that we mention above on 60/40. Obviously, the patterns of the new schedule will effect money flow quite a bit so modelling will be critical.
Some other areas where funding change will happen in the name of alignment on the GP narrative will be:
- PHN funding – this is a separate op-ed on its own, but PHNs are a good idea badly executed with short-term ineffective funding today;
- Mental health funding – GPs deal with the most mental health load and aren’t funded to do it, especially the complex stuff – see also blended funding;
- Aged care funding – see also blended funding;
- And more: note carefully, we have not gone to state funding for primary care with a view to connecting general practice properly to community care and hospitals which is a huge topic we touch on below.
Funding is huge and complex and I’ve got another seven items I could put here. The above is just a taste.
The timing of all this?
Huge question to be sorted and it needs to be because you can’t plan and do business if you don’t have a timetable for change.
2. The states and the National Health Reform Agreement
This probably could have taken the No 1 spot on this list if we were doing priority. It’s at once potentially the most important and the most troubling thing on this listicle.
How does the federal government convince the states to stop kicking the can down the road on their terminal and obsessive plans to build out more hospital infrastructure, get these vital acute care institutions to talk properly to the community via primary care, and really set in motion the narrative that GPs should be set up properly to manage chronic care in the community to prevent system meltdown via hospital system failure at scale?
Here are the most important lines of what the National Health Reform Agreement (NHRA) is meant to do:
[Improve] “health outcomes for Australians, by providing better coordinated and joined up care in the community, and ensuring the future sustainability of Australia’s health system” (our emphasis).
Jeez, are the states reading this one sentence and thinking it through seriously?
If anything, this sentence isn’t contemplating hospitals enough – but maybe that’s the point.
Here’s the big problem for any GP out there who wants to get active in any way they can on this vital five-year planning document for the national healthcare system:
- The quoted sentence above isn’t in play today if you look at what a binfire hospitals are in each state as things stand;
- States aren’t funded to do what that sentence says they should be doing – they are funded to run hospitals and things won’t change until there is much better nuance in how the states contribute to effective community health;
- People working in hospitals are as great and committed as GPs and maybe even more under the gun in terms of prospects for meaningful reform that will make their lives better – they are busy day-to-day putting fires out and need support, help and understanding.
A year or so ago the NHRA was on some sort of track to start addressing the sentence quoted above for the first time in the history of the agreement. States are bleeding money, and they want in on a solution for healthcare system efficiency and cost so they were aligning with the Commonwealth on the “big whiteboard plan” for change.
Then, possibly very unwisely, the federal government decided to tie foundational supports for the NDIS to the NHRA and a few key people in the NHRA negotiation process left and we lost continuity in the planning.
Word is, everything has stopped and gone backwards towards nothing much happening.
This last point, if it plays out, will be a disaster for meaningful reform and GPs. The NDIS thing is one of the symptoms of trying to pack in too much reform too quickly.
If GP advocacy groups could do one thing for the next few months it would be to somehow break into this process and politely try to help the powers that be get the NHRA back on track.
If we get the usual financial agreement, rather than much needed funding and policy paradigm changes, a lot of momentum in the push to transform the system to weight it far more into management in the community will be lost for another five years.
3. Sharing by default
A lot of GPs still won’t know and won’t care what “sharing by default” is, but they should by now.
It’s a massive program of healthcare system technology infrastructure change being driven by DoDHA (and the Australian Digital Health Agency) with the aim of being able to share meaningful patient data between providers, and between providers and patients, in near real-time.
The program is huge, complex and will likely be expensive and fraught with problems, but the extensive planning and goals are all well thought out and things are starting to happen.
One thing that could happen is that GPs will be able to properly talk to hospitals, specialists and relevant allied health providers about meaningful patient plans in near real-time. It almost sounds like science fiction if you’re a GP reading this and listening to that heart-warming ping and hum of your fax still in the background.
The hope here is that GPs don’t have to suffer that much change at all and your PMS magically iterates under you so you don’t notice that much, other than you are far more connected and find it much easier to collaborate with provider peers and your patients.
It probably won’t happen like this but it probably will happen in time.
The Commonwealth is pushing sharing by default as a big first step in its grand whiteboard plan because you can’t do blended funding unless you have better data and data sharing.
Data sharing and a cloud-enabled technology base will enable everyone to measure and manage how blended funding is targeted. From a timetable perspective it means the funding changes will flow more later than sooner, but don’t be fooled, the changes will happen within the six-year runway.
One more thing which I’m sure is another potboiler management book which I haven’t read yet: it’s not the technology, stupid.
The technology is all there, it’s working in other countries big-time. Yep, we can stuff up the execution – we’re pretty good at that – but we should get there this time eventually because there’s a good roadmap and a well thought out plan, which there wasn’t when the government first thought of and built the My Health Record.
Again, don’t get too distracted with technology. The change is all about organisational culture and people (and mice and cheese of course) and that’s where GP groups can get involved and start thinking a lot more about how to help.
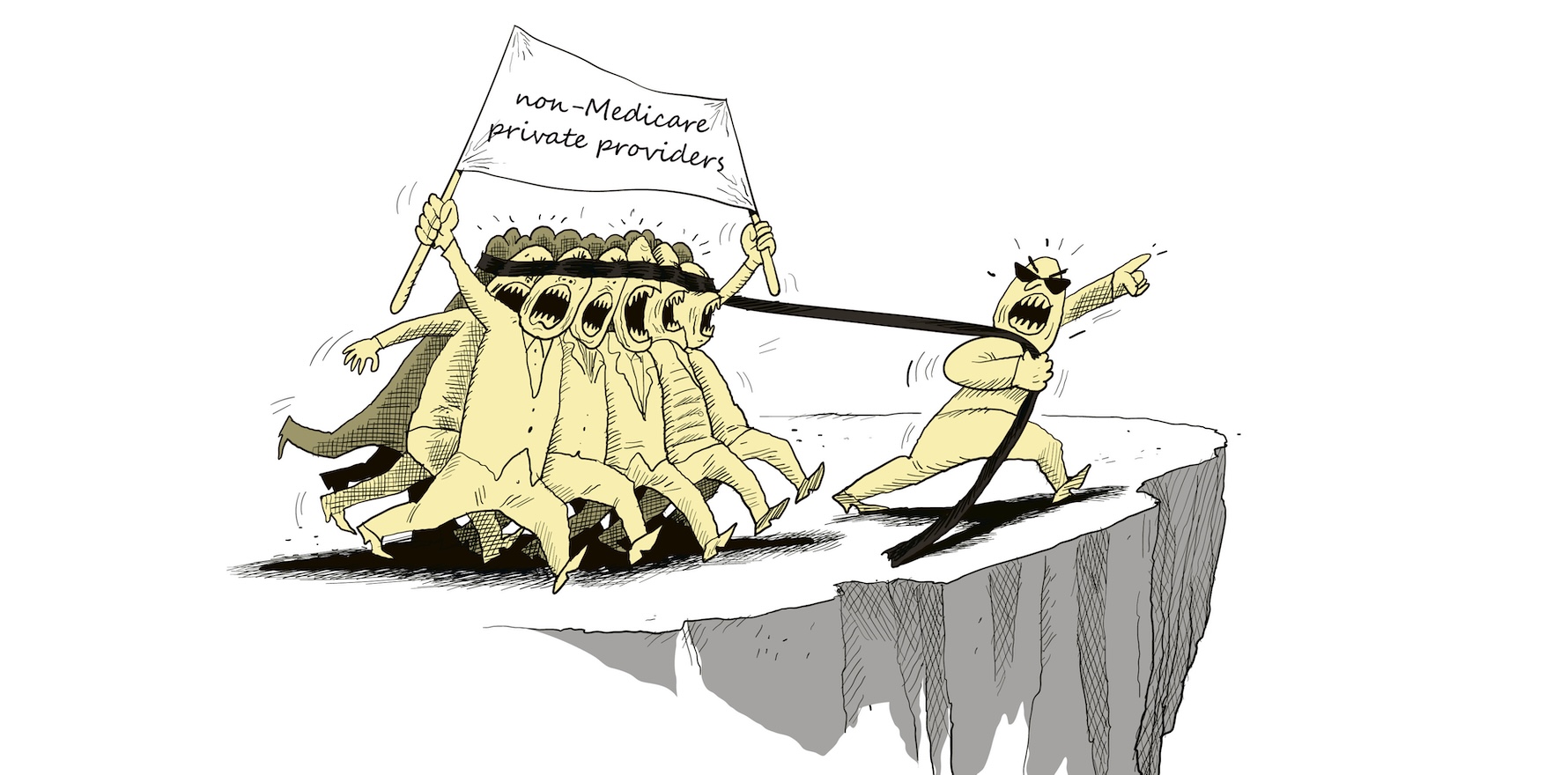
4. The rapidly expanding non-Medicare healthcare system and economy
An unusual dynamic about GPs that I’ve observed is that when in conversation about the system and reform they never seem to see themselves as a part of the private healthcare system.
That’s of course those nasty obscenely profitable and conniving private health insurers, the once voracious and now humbled private hospital sector, and increasingly, the rapidly growing non-Medicare telehealth platform providers like Eucalyptus, Mosh, Instant Scripts, Midnight Health and so forth.
Many GPs even will distinguish themselves from the big corporates.
ForHealth, one of our two largest corporates, and growing again fast these days, is the essence of private – it’s a private equity play and as such, many see this as a big worry, especially given the Healthscope debacle.
Private money of course is private money. PE money is just private money at scale, and sometimes, better organised – in the case of Healthscope of course, sometimes it’s not.
GPs are part of the private healthcare economy. They are mostly all private businesses that need to make a profit – a small few are not-for-profits and that’s another interesting story – just like Sonic, ForHealth and Medibank.
Going forward, however, a big change is that they are part of the rapid build-out of the non-Medicare economy. Thanks, Associate Professor Karen Price, who started the trend as president of the RACGP in 2019 by saying GPs will go broke unless they start mixed billing.
This week at the One Health Summit she doubled down by saying we will never get to 90% bulk billing – and we probably shouldn’t – because the reality is that lots of patients can afford to pay above the MBS rebate for their GP and they probably should to make the system mix more efficient.
She qualified her argument of course by reinforcing that the bulk-billing safety net was a vital part of the system and will remain a vital part and that GPs needed to use it even in high socioeconomic areas when it is needed.
How does this all change things moving forward for GPs?
In a few interesting ways:
- If you think about all the expanding options to work as a GP going forward, a lot of it is in this non-Medicare economy. If you want variety in the future you’re going to get it: work in a UCC (actually this is more block-funded Medicare, not private), work for telehealth platform part-time, work a couple days in a traditional bricks-and-mortar practice doing mixed billing, forget all your worries about tax, business, policy and the like and work for a decent corporate, work in a new state-run “integrated healthcare hub” with a healthcare team onsite, work for a private health insurer with a level of vertical integration to increase your impact, prescribe cannabis if you want too (maybe they’ll fix this). In short, variety and flexibility are coming.
- Mixed billing, six years of the one government committed to GPs and GP funding, and remuneration will at the very least be better than it has been for the past decade or so via Medicare, with the private economy topping things up.
- The “sharing by default” technology stack, being almost wholly cloud focused, is going to make innovation in general practice a lot easier and more accessible – I think. That’s going to make starting new models of care in GPs’ own businesses potentially a lot easier. But the main thing it should do is significantly decrease GP isolation from the rest of the system. GPs should be much better connected in virtual care teams, with hospitals and with relevant local allied health providers. Being a GP should mean you can achieve a lot more impact in your community.
- Unchecked, the non Medicare ecosystem will naturally tend to fragment care in ways that aren’t good – that, of course, is a downside that needs thought.
An interesting side note on the non-Medicare economy: because it’s expanding so rapidly – a lot via new virtual technology offerings – it increasingly makes large parts of the health journey of patients invisible to government.
When Medicare ruled the waves the government could see enough to manage the system and the patient, moderate change and keep a close eye on continuity of care.
The rapid rise of the non-Medicare economy is threatening the important ability for oversight and management of system wide levers to maintain and build continuity of care.
So, expect the government in the not-too-distant future to introduce regulation and legislation that somehow captures this fascinating, innovative, at times wild and dangerous, and rapidly expanding part of our healthcare system, back into the purview of government, with a key goal of maintaining and improving continuity of care, and especially connectivity with the Medicare economy.
How they are going to do this and when? That’s for another article, of course.
Okay, that’s it for this week, if you even made it this far.
Next week we look at the tax system (state and federal), education and training, scope of practice, and workforce and AI.
Note: All of these topics will be part of Burning GP 2.0 which we are planning for October of 2026. If you want in, you can email me with your ideas at jeremy@medical republic.com.au, and cc talia@medicalrepublic.com.au.